Type I NSTEMI Management & Transfusion Medicine
C H E S T P A I N
PEARLS OF THE DAY:
1. ACS algorithm & medical management of a type I NSTEMI
2. PRBC transfusion thresholds in patients with cardiovascular disease
3. Five landmark trials on the topic of transfusion
3. Five landmark trials on the topic of transfusion
Dr. Armstrong presented an elderly female patient with NHL, and a recent positive NM stress test. In light of the patient's active malignancy with impressive leukocytosis (WBC: 134), she was not a candidate for coronary angiogram/PCI.
Subsequently, she presented to PPMC with chest pain and was found to have a type I NSTEMI (anginal CP + positive biomarkers without ST changes on EKG).
ACS ALGORITHM:
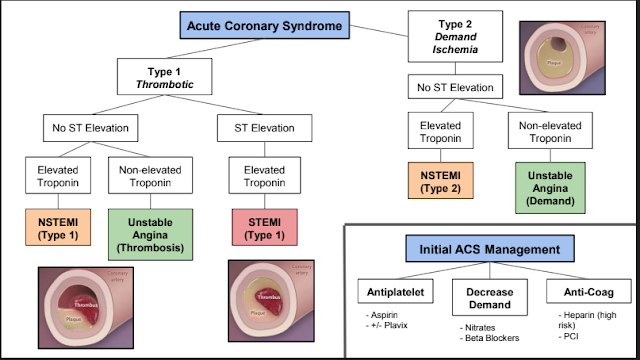
Algorithm c/o Brandon Temte
Our patient fell into the type I NSTEMI category. Her TIMI score was 4. Of course, standard therapy in this patient would advise coronary cath +/- PCI. This patient was not a candidate for cath due to her NHL with profound leukocytosis and so she had to be managed medically.
To review: medical management for Type I ACS includes: Aspirin + P2Y12 inhibitor + anticoagulation.
Ezra et. al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes: Executive Summary. J Am Coll Cardiol. 2014 Dec, 64 (24) 2645-2687.
As a complication of the anticoagulation & anti-platelet therapy, the patient subsequently developed acute blood loss anemia and a hemothorax. The patient received PRBCs & a transfusion threshold of HGB > 9 was used in the setting of ACS
Clinical Question:
Dr. Armstrong investigated the data regarding the transfusion threshold for patients with anemia and underlying CAD.
Effect of restrictive versus liberal transfusion strategies on outcomes in patients with cardiovascular disease in a non-cardiac surgery setting: systematic review and meta-analysis. BMJ 2016; 352 doi: https://doi.org/10.1136/bmj.i1351 (Published 29 March 2016). https://www.bmj.com/content/352/bmj.i1351
The study reviewed and evaluated 11 trials.
The meta analysis demonstrated a trend toward a lower rate of cardiovascular events in patients managed with more liberal transfusion thresholds.
Of note: TRICS III came out after the above BMJ meta analysis and again found that a strict threshold is non inferior to a liberal threshold.
TRICS III (2017): Mazer CD, et al. "Restrictive or Liberal Red-Cell Transfusion for Cardiac Surgery". The New England Journal of Medicine. 2017. 377(22):2133-44.
- Clinical Question: In patients undergoing cardiac surgery who have a moderate-to-high risk of death, is a restrictive transfusion strategy applied throughout the perioperative period noninferior to a liberal transfusion strategy, in terms of major morbidities and mortality?
- Bottom Line: A restrictive red-cell transfusion strategy (transfusing for hemoglobin <7.5 g/dL) resulted in fewer red-cell transfusions than a more liberal red-cell transfusion strategy (hemoglobin <9.5 g/dL) and was non-inferior for major clinical outcomes among moderate- and high-risk patients undergoing on-pump cardiac surgery.
The landmark trials regarding transfusion threshold are:
(information c/o https://www.wikijournalclub.org/wiki/WikiJournalClub:Usable_articles#Hematology)
FOCUS (2011): Carson JL, et al. "Liberal or Restrictive Transfusion in High-Risk Patients after Hip Surgery". The New England Journal of Medicine. 2011. 365(26):2453-62.
- Clinical Question: Among high-risk patients undergoing hip surgery, does a liberal transfusion strategy (target hemoglobin >10 g/dL) improve survival or functional outcomes at 60 days compared to a restrictive strategy (target hemoglobin >8 g/dL)?
- Bottom Line: Among high-risk patients undergoing hip surgery, a liberal transfusion strategy targeting a hemoglobin >10 g/dL does not improve survival or functional outcomes compared to a restrictive strategy targeting a hemoglobin of >8 g/dL.
TRISS (2014): Holst L, et al. "Transfusion thresholds in Septic Shock". The New England Journal of Medicine. 2014. 371(15):1381-1391.
- Clinical Question: In patients with septic shock, how does a restrictive transfusion strategy (Hgb ≤ 7 g/dL) compare with a liberal transfusion strategy (Hgb ≤ 9 g/dL) in terms of 90-day mortalit
- Bottom Line: Patients with septic shock who underwent transfusion at a Hgb threshold of 7 g/dL had similar mortality at 90 days but used 50% fewer units of blood compared with those who underwent transfusion at a Hgb threshold of 9 g/dL.
TRICC (1999): Hebert PC, et al. "A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care". The New England Journal of Medicine. 1999. 340(6):409-417.
- Clinical Question: Among critically ill patients, how does a restrictive transfusion strategy (hemoglobin goal of 7-9 g/dL) compare with a liberal transfusion strategy (hemoglobin goal of 10-12 g/dL) in decreasing mortality?
- Bottom Line: In critically ill patients, restrictive transfusion (Hgb >7 g/dL) is associated with better survival compared to liberal strategy (Hgb >10).
Transfusion strategies for acute upper gastrointestinal bleeding (2013): Villanueva C et al. "Transfusion strategies for acute upper gastrointestinal bleeding". The New England Journal of Medicine. 2013. 368(1):11-21.
- Clinical Question: In patients with an upper GI bleed, how does a restrictive transfusion goal compare with a liberal transfusion goal in regards to mortality?
- Bottom Line: Among patients with acute upper GI bleeding, a restrictive transfusion threshold (Hgb ≥7) was associated with reduced mortality at 45 days compared to a liberal transfusion threshold (Hgb ≥10).
Thanks for reading, Emma
The information posted above is for educational use only by the trainees of a non-profit hospital residency program.




Comments
Post a Comment